Cardiac cycle
Cardiac cycle
The cardiac cycle refers to a complete heartbeat from its generation to the beginning of the next beat, and so includes the diastole, the systole, and the intervening pause. The frequency of the cardiac cycle is described by the heart rate, which is typically expressed as beats per minute. Each beat of the heart involves five major stages. The first two stages, often considered together as the “ventricular filling” stage, involve the movement of blood from the atria into the ventricles. The next three stages involve the movement of blood from the ventricles to the pulmonary artery (in the case of the right ventricle) and the aorta (in the case of the left ventricle).
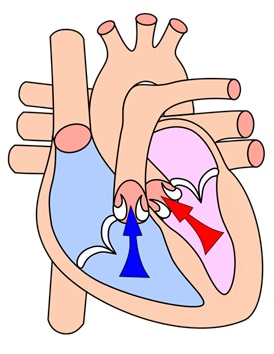
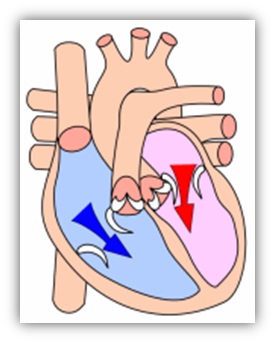
The first stage, “early diastole,” is when the semilunar valves (the pulmonary valve and the aortic valve) close, the atrioventricular (AV) valves (the mitral valve and the tricuspid valve) open, and the whole heart is relaxed. The second stage, “atrial systole,” is when the atrium contracts, and blood flows from atrium to the ventricle. The third stage, “isovolumic contraction” is when the ventricles begin to contract, the AV and semilunar valves close, and there is no change in volume. The fourth stage, “ventricular ejection,” is when the ventricles are contracting and emptying, and the semilunar valves are open. During the fifth stage, “isovolumic relaxation time”, pressure decreases, no blood enters the ventricles, the ventricles stop contracting and begin to relax, and the semilunar valves close due to the pressure of blood in the aorta.
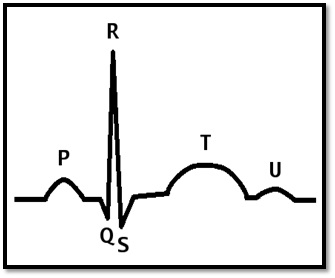
Throughout the cardiac cycle, blood pressure increases and decreases. The cardiac cycle is coordinated by a series of electrical impulses that are produced by specialised pacemaker cells found within the sinoatrial node and the atrioventricular node. The cardiac muscle is composed of myocytes which initiate their own contraction without the help of external nerves (with the exception of modifying the heart rate due to metabolic demand). Under normal circumstances, each cycle takes 0.8 seconds.
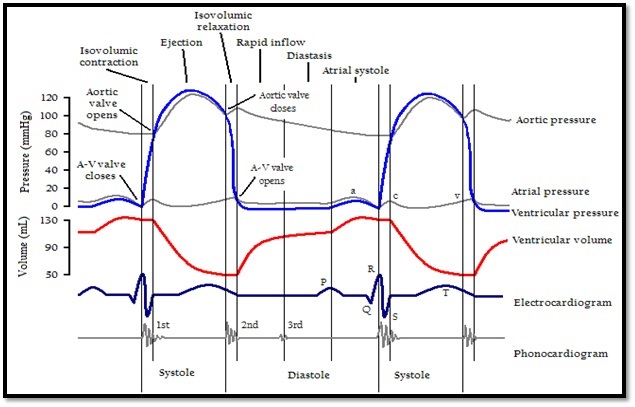
Cardiac events occurring in the cardiac cycle. Two complete cycles are illustrated. |
Physiology
The heart is a four-chambered organ consisting of right and left halves. The upper two chambers, the left and right atria, are entry-points into the heart, while the lower two chambers, the left and right ventricles, are responsible for contractions that send the blood through the circulation. The circulation is split into the pulmonary and systemic circulation. The role of the right ventricle is to pump deoxygenated blood to the lungs through the pulmonary trunk and pulmonary arteries. The role of the left ventricle is to pump newly oxygenated blood to the body through the aorta.
Rhythmical conduction
Cardiac muscle has automaticity, which means that it is self-exciting. The muscle contractions are myogenic, or generated by the muscle cell itself. This is in contrast with skeletal muscle, which requires nervous stimuli (either conscious or reflex) for excitation. The heart’s rhythmic contractions occur spontaneously, although the rate of contraction can be changed by nervous or hormonal influences. For example, the sympathetic nerve accelerates heart rate and the vagus nerve decelerates the heart rate.
The rhythmic sequence of contractions (sinus rhythm), is coordinated by the sinoatrial (SA) and atrioventricular (AV) nodes. The sinoatrial node, often known as the cardiac pacemaker, is located in the upper wall of the right atrium and is responsible for the wave of electrical stimulation that initiates atrial contraction by creating an action potential. Once the wave reaches the AV node, situated in the lower right atrium, it is delayed there before being conducted through the bundles of His and back up the Purkinje fibers, leading to a contraction of the ventricles. The delay at the AV node allows enough time for all of the blood in the atria to fill their respective ventricles. In the event of severe pathology, the AV node can also act as a pacemaker; this is usually not the case because their rate of spontaneous firing is considerably lower than that of the pacemaker cells in the SA node and hence is overridden.
Stages
The following is a summary of the cardiac cycle;
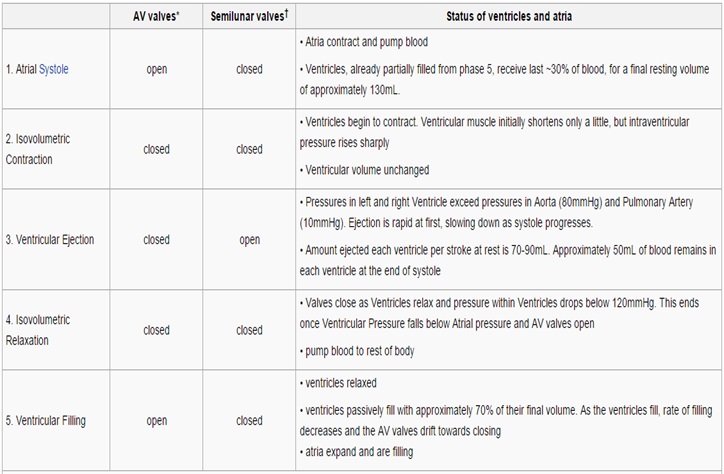
Atrial systole
Atrial systole is the contraction of the atrial syncytium of cardiac muscle cells of the left and right atria, following electrical stimulation. This conduction takes place via the gap junctions of the connecting intercalated discs. Normally, both atria contract at the same time. The term systole is synonymous with contraction (movement or shortening) of a muscle. Electrical systole is the electrical activity that stimulates the cardiac muscle of the heart chambers to make them contract. This is soon followed by mechanical systole, which is the mechanical contraction of the heart.
As the atria contract, the blood pressure in each atrium increases, forcing additional blood into the ventricles. The additional flow of blood is called atrial kick.
80% of the blood flows passively down to the ventricles, so the atria do not have to contract a great amount.
Atrial kick is absent if there is loss of normal electrical conduction in the heart, such as during atrial fibrillation, atrial flutter, and complete heart block. Atrial kick is also different in character depending on the condition of the heart, such as stiff heart, which is found in patients with diastolic dysfunction.
Atrial systole, also known as auricular systole due to the contraction of the two auricles of the heart, takes approximately 0.1 seconds.
Detection
Electrical systole of the atria begins with the onset of the P wave on the ECG. The wave of bipolarization (or depolarization) that stimulates both atria to contract at the same time is due to sinoatrial node which is located on the upper wall of the right atrium.the sinoatrial node can be detected by catheterization.
Ventricular systole
Ventricular systole is the contraction of the ventricular syncytium of cardiac muscle cells of the left and right ventricles, following electrical stimulation. This conduction takes place via the gap junctions of the connecting intercalated discs.
At the later part of the ejection phase, although the ventricular pressure falls below the aortic pressure, the aortic valve remains open because of the inertial energy of the ejected blood.
The graph of aortic pressure throughout the cardiac cycle displays a small dip (the “incisure” or “dicrotic notch”) which coincides with the aortic valve closure. The dip in the graph is immediately followed by a brief rise (the “dicrotic wave”) then gradual decline. Just as the ventricles enter into diastole, the brief reversal of flow from the aorta back toward the left ventricle causes the aortic valves to shut. This results in the slight increase in aortic pressure caused by the elastic recoil of the semilunar valves and aorta.
The total volume of blood remaining in the ventricle just at the end of the ventricular contraction is called end-systolic volume (ESV).
Assuming a pulse of 72 beats per minutes, ventricular systole takes 0.3 seconds to complete
Detection
Heart sounds
The closing of the mitral and tricuspid valves (known together as the atrioventricular valves) at the beginning of ventricular systole cause the first part (the lubb) of the “lubb-dubb” sound made by the heart as it beats. Formally, this sound is known as the first heart sound, or S1. This first heart sound is created by the closure of the mitral and tricuspid valves and is actually a two component sound, M1, T1.
The second part (the dubb) of the “lubb-dubb” (the second heart sound, or S2), is caused by the closure of the aortic and pulmonary valves at the end of ventricular systole. As the left ventricle empties, its pressure falls below the pressure in the aorta, and the aortic valve closes. Similarly, as the pressure in the right ventricle falls below the pressure in the pulmonary artery, the pulmonary valve closes. The second heart sound is also two components, A2 and P2. The aortic valve closes earlier than the pulmonary valve and they are audibly separated from each other in the second heart sound. This “splitting” of S2 is only audible during inhalation. However, some cardiac conduction abnormalities such as left bundle branch block (LBBB) allow the P2 sound to be heard before the A2 sound during expiration. With LBBB, inhalation brings A2 and P2 closer together where they cannot be audibly distinguished.
Electrocardiogram
In an electrocardiogram, electrical systole of the ventricles begins at the beginning of the QRS complex.
Diastole
Cardiac diastole is the period of time when the heart relaxes after contraction in preparation for refilling with circulating blood. Ventricular diastole is when the ventricles are relaxing, while atrial diastole is when the atria are relaxing. Together they are known as complete cardiac diastole.
During ventricular diastole, the pressure in the (left and right) ventricles drops from the peak that it reaches in systole. When the pressure in the left ventricle drops to below the pressure in the left atrium, the mitral valve opens, and the left ventricle fills with blood that was accumulating in the left atrium. The isovolumic relaxation time (IVRT) is the interval from the aortic component of the second heart sound, that is, closure of the aortic valve, to onset of filling by opening of the mitral valve. Likewise, when the pressure in the right ventricle drops below that in the right atrium, the tricuspid valve opens, and the right ventricle fills with blood that was accumulating in the right atrium. During diastole the pressure within the left ventricle is lower than that in aorta, allowing blood to circulate in the heart itself via the coronary arteries.
References
wikipedia:https://en.wikipedia.org/wiki/Cardiac_cycle
اسم الطالب
صفاء فاضل علي
المرحلة الاولى